[1] The need for standardized MRI meta-analyses in epilepsy
Epilepsy is a neurological disorder characterized by an enduring predisposition to generate epileptic seizures. The disorder may be defined by any of the following: (1) at least two unprovoked seizures occurring more than 24 hours apart; (2) one unprovoked seizure, with a high probability (>60%) of additional, recurrent seizures; (3) diagnosis of an epilepsy syndrome, even if the risk of further seizures is low (for example, benign epilepsy with centro-temporal spikes, BECTS)3. The International League Against Epilepsy (ILAE) has formally delineated several classifications of seizures and epilepsy sub-types. These classifications have been revised from earlier definitions (see: ILAE reports from 1981 and 1989) in order to improve our organization of recognized forms of epilepsy and facilitate identification of new forms of the disorder. Despite amending these terminologies to include electroclinical characteristics, structural lesions and metabolic abnormalities, our understanding of the neurobiological processes contributing towards, and occurring as a consequence of, epilepsy often remains unclear.
Advances in magnetic resonance imaging (MRI) have helped clinical epileptologists and research scientists study the structure and function of the living human brain in epilepsy in unprecedented detail. For clinicians, neuroimaging now plays a crucial role in neurosurgical planning5, localization of the epileptic area6 and identification of underlying hippocampal sclerosis, tumors or malformations of cortical development7 in epileptic disorders. For research scientists, MRI has allowed us to scan relatively small (N=10-100) groups of epilepsy patients and healthy controls and then fit statistical models to these scans in order to probe factors that broadly affect neuroanatomy and function in the disorder8. Although these studies have identified numerous structural and functional abnormalities possibly associated with the underlying pathology, their modest statistical power typically leads to inconsistent findings from one investigation to the next – overall limiting our ability to reliably generalize any neurobiological insights to the wider population of people with epilepsy.
Some groups have employed systematic reviews, or meta-analyses, of previous neuroimaging studies in order to address these inconsistencies. In these meta-analyses, findings from several independent MRI investigations are reviewed and quantified using ‘random’ and ‘mixed-effects’ statistical models in order to provide more reliable illustrations of underlying biology. Although several meta-analyses have successfully identified more consistent patterns of gray matter atrophy9, gray matter hypertrophy10 and microstructural white matter alteration11 in epilepsy, they still base their findings on summary statistics from small neuroimaging studies that vary greatly with respect to the processing algorithms and statistical models used on their respective individual datasets. This likely contributes towards confounding inflations of any observed effects, potential ‘blurring’ of more subtle effects, and possible discrepancies from one meta-analysis to the next12.
The ENIGMA model of MRI meta-analysis, whereby several independent research groups conduct harmonized neuroimaging analyses on their respective collections of MRI scans, may overcome previous limitations of the meta-analytical paradigm. The ENIGMA model combines important quantitative measures of brain shape, volume and wiring from international research centres, with each centre analysing their own MRI data using identical, standardized protocols. These protocols, which are all freely available online, facilitate efficient analysis of MRI data on large datasets (e.g. up to 31,000 subjects – 79% healthy controls, 21% psychiatric/neurological patients) and have previously been applied in landmark studies of the hippocampus (published in Nature Genetics, 2012), white matter degeneration (published in NeuroImage, 2013) and subcortical brain structures (published in Nature, 2015). This meta-analytic approach may yield sufficient statistical power to robustly and reliably explore neurobiological substrates of epilepsy that no individual site could detect on its own.
[2] ENIGMA-Epilepsy: Overview, aims & objectives
The ENIGMA-Epilepsy collaboration follows on from other ongoing disease-based ENIGMA working groups such as ENIGMA-schizophrenia, ENIGMA-bipolar, ENIGMA-major depressive disorder, ENIGMA-addiction, ENIGMA-ADD, ENIGMA-HIV, ENIGMA-OCD, ENIGMA-PTSD, and ENIGMA-22q11DS. A broad overview of the ENIGMA-Epilepsy is provided below:
-
STAGE 1: Collaborations are formed between epilepsy centers; centers are invited to join ENIGMA-Epilepsy
-
STAGE 2: Neuroimaging analysis protocols are circulated to each epilepsy center
-
STAGE 3: Analysts at each centre generate a series of standardized statistical models in order to extract summary measures (p-values, z-scores, etc.) quantifying differences in the volume, shape and wiring of various brain structures in people with epilepsy and healthy controls. N.B.: Summary measures are fully anonymized.
-
STAGE 4: Summary measures are forwarded to a central meta-analysis site, where they undergo fixed-effects meta-analysis. Meta-analysis may reveal patterns of gray matter damage or white matter loss in particular pre-specified groups of people with epilepsy when compared to neurologically healthy controls.
The overarching aim of the ENIGMA-EPILEPSY collaboration is be to improve our understanding of in vivo neuroanatomical disruptions in people with epilepsy compared to the general population. Other important objectives of the collaboration include:
-
To create a worldwide network of epilepsy neuroimaging centres.
-
To collect summary statistics on brain shape, brain volume and brain wiring from thousands of people with epilepsy and thousands of neurologically healthy control participants in order to vastly improve the statistical power of neuroimaging research.
-
To compare and contrast these measures in affected/unaffected groups and, accordingly, illustrate possible differences between the two.
-
To identify structural differences between the major forms of epilepsy and major types of seizure.
-
To develop collaborations and infrastructure for future analyses
[3] Overview of ENIGMA-Epilepsy project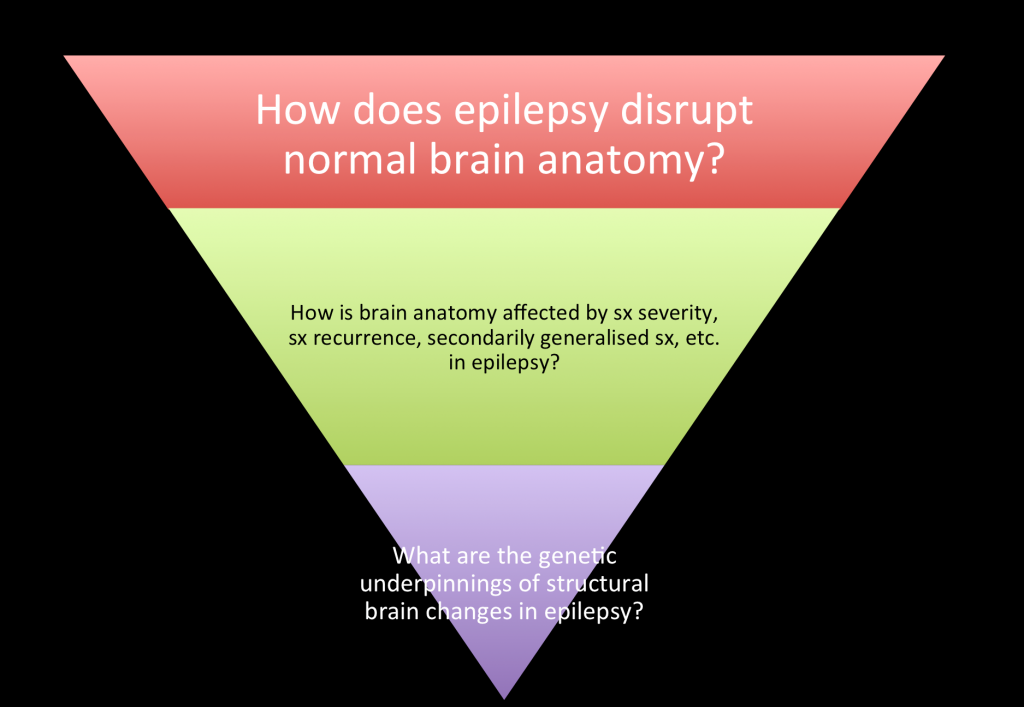
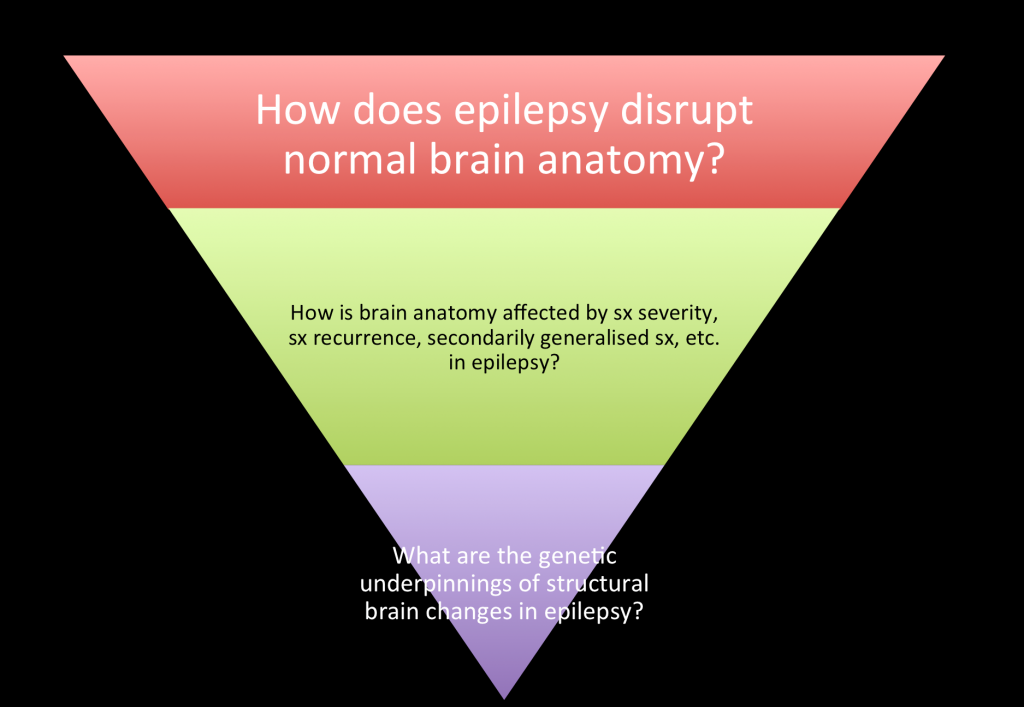
ENIGMA-Epilepsy will take its lead from other ENIGMA working groups by commencing with simpler research questions that eventually progress into more complex investigations. For example, we will start by asking the relatively straightforward question, “In what way does epilepsy disrupt normal brain anatomy?” From here, we will gradually progress onto more specific questions, such as, “Is there a structural basis to secondary seizure generalization?” or, “What common genetic variants are associated with disrupted brain anatomy in epilepsy?”
There are currently two ongoing ENIGMA-Epilepsy research projects. The first is using T1-weighted structural MR images to examine structural variations in gray matter volume, whereas the second is using diffusion tensor imaging (DTI) to study variations in microstructural white matter integrity.
[4] Project 1: ENIGMA-Epilepsy VOLUMETRICS
In ENIGMA-Epilepsy VOLUMETRICS, we will compare variations in normal cortical and subcortical gray matter volumes between a phenotypically heterogeneous group of people with epilepsy and a group of neurologically healthy controls. Previous investigations of gray matter volume (GMV) have indicated a variety of volumetric alterations in epilepsy; from GMV increases in the bilateral medial frontal gyrus / anterior cingulate and GMV reductions in the bilateral thalamus of juvenile myoclonic epilepsy patients10 to GMV reductions in the bilateral thalamus and ipsilateral mesial temporal structures in temporal lobe epilepsy9. These observations are strongly supported by cellular investigations, which have illustrated a central role for thalamic reticular neurons in loss of consciousness during seizures13 and significant modulations of hippocampal structure in experimental animal models of epilepsy14-16.
We will first examine epilepsy as a whole – testing the hypothesis that all epilepsy is characterized by distinct alterations of GMV in the thalamocortical and mesiotemporal brain regions when compared to neurologically healthy controls. Follow-up analyses may explore more specific patterns of GM variation in large sub-groups of epilepsy patients; e.g. focal epilepsies, generalized epilepsies and mesial temporal lobe epilepsy.
All gray matter volumes will be extracted using FreeSurfer – a standardized software suite used to extract cortical and subcortical volumes and surface area measures. ENIGMA FreeSurfer protocols employed as part of the group’s Nature Genetics (2012) and Nature (2015) papers are available from the following location: http://enigma.ini.usc.edu/protocols/imaging-protocols/extract-volume-values/
[5] Project 2: ENIGMA-Epilepsy DTI
In ENIGMA-Epilepsy DTI, we will investigate voxelwise white matter (WM) variation in a phenotypically heterogeneous group of people with epilepsy compared to a group of neurologically healthy controls. Previous DTI studies have illustrated microstructural disruptions in the majority of WM tracts for people with temporal lobe epilepsy17, with the most profound changes occurring ipsilateral to the side of seizure onset, close to the seizure onset zone. Previous DTI investigations have also revealed significant impairments of the thalamocortical circuitry in juvenile myoclonic epilepsy18, childhood absence epilepsy19 and idiopathic generalized epilepsy20. Cellular studies have similarly implicated the thalamocortical circuitry in the generation of spike-wave seizures, which are a common feature of generalized epilepsy21.
Similar to ENIGMA-Epilepsy VOLUMETRICS, ENIGMA-Epilepsy DTI will initially consider WM changes in people with epilepsy as a whole – testing the hypothesis that people with epilepsy have widespread disruptions of the white matter skeleton when compared to neurologically healthy controls. Follow-up analyses may explore more specific patterns of WM alteration in sub-groups of epilepsy patients; e.g. focal epilepsies, generalized epilepsies and mesial temporal lobe epilepsy, all in large numbers of patients.
White matter organization will be assessed using Tract-Based Spatial Statistics (TBSS). TBSS is a component of the standardized FSL software package. It is used to analyze diffusion-weighted MRI scans, measuring the anisotropic diffusion of water in various white matter tracts and indirectly providing indices of microstructural impairment (fractional anisotropy, mean diffusion, axial diffusivity, radial diffusivity, etc.). TBSS protocols employed as part of ENIGMA’s 2013 NeuroImage paper are available at: http://enigma.ini.usc.edu/protocols/dti-protocols/
[6] ‘Phase II’ [2016-]
Our two inaugural projects – ENIGMA-Epilepsy: Volumetrics and ENIGMA-Epilepsy: DTI – will serve as important starting points for future collaborations testing more specific hypotheses related to disease chronicity, drug resistance and genetic predisposition in epilepsy. We hope to develop more explicit research questions for phase 2 of ENIGMA-Epilepsy once an initial framework for collaborative research is fully in place.
[7] References
-
Stein, J. L. et al. Identification of common variants associated with human hippocampal and intracranial volumes. Nature Genetics 44, 552–561 (2012).
-
Hibar, D. P. et al. Common genetic variants influence human subcortical brain structures. Nature (2015). doi:10.1038/nature14101
-
Fisher, R. S. et al. ILAE Official Report: A practical clinical definition of epilepsy. Epilepsia 55, 475–482 (2014).
-
Berg, A. T. et al. Revised terminology and concepts for organization of seizures and epilepsies: report of the ILAE Commission on Classification and Terminology, 2005-2009. Epilepsia 51, 676–685 (2010).
-
Siegel, A. M. et al. Medically Intractable, Localization‐related Epilepsy with Normal MRI: Presurgical Evaluation and Surgical Outcome in 43 Patients. Epilepsia 42, 883–888 (2001).
-
Spencer, S. S. The Relative Contributions of MRI, SPECT, and PET Imaging in Epilepsy. Epilepsia 35, S72–S89 (1994).
-
RI, K. & RC, K. Neuroimaging of epilepsy. Semin Neurol 22, 279–288 (2002).
-
Thompson, P. M. et al. The ENIGMA Consortium: large-scale collaborative analyses of neuroimaging and genetic data. Brain Imaging and Behavior 8, 153–182 (2014).
-
Li, J., Zhang, Z. & Shang, H. A meta-analysis of voxel-based morphometry studies on unilateral refractory temporal lobe epilepsy. Epilepsy Research 98, 97–103 (2012).
-
Cao, B. et al. A meta-analysis of voxel-based morphometry studies on gray matter volume alteration in juvenile myoclonic epilepsy. Epilepsy Research 106, 370–377 (2013).
-
Otte, W. M., Sander, J. W., Duncan, J. S., Dijkhuizen, R. M. & Braun, K. P. J. A meta‐analysis of white matter changes in temporal lobe epilepsy as studied with diffusion tensor imaging. Epilepsia 53, 659–667 (2012).
-
Seneviratne, U., Cook, M. & D’Souza, W. Focal abnormalities in idiopathic generalized epilepsy: A critical review of the literature. Epilepsia 55, 1157–1169 (2014).
-
Steriade, M. Sleep, epilepsy and thalamic reticular inhibitory neurons. Trends in Neurosciences 28, 317–324 (2005).
-
Sloviter, R. S. Decreased hippocampal inhibition and a selective loss of interneurons in experimental epilepsy. Science 235, 73–76 (1987).
-
Furshpan, E. J. & Potter, D. D. Seizure-like activity and cellular damage in rat hippocampal neurons in cell culture. Neuron 3, 199–207 (1989).
-
Sloviter, R. S. Permanently altered hippocampal structure, excitability, and inhibition after experimental status epilepticus in the rat: The ‘dormant basket cell’ hypothesis and its possible relevance to temporal lobe epilepsy. Hippocampus 1, 41–66 (1991).
-
Otte, W. M. et al. A meta-analysis of white matter changes in temporal lobe epilepsy as studied with diffusion tensor imaging. Epilepsia 53, 659–667 (2012).
-
Deppe, M. et al. Nerve fiber impairment of anterior thalamocortical circuitry in juvenile myoclonic epilepsy. Neurology 71, 1981–1985 (2008).
-
Yang, T. et al. White matter impairment in the basal ganglia-thalamocortical circuit of drug-naïve childhood absence epilepsy. Epilepsy Research 99, 267–273 (2012).
-
Groppa, S. et al. White matter microstructural changes of thalamocortical networks in photosensitivity and idiopathic generalized epilepsy. Epilepsia 53, 668–676 (2012).
-
Blumenfeld, H. Cellular and Network Mechanisms of Spike‐Wave Seizures. Epilepsia 46, 21–33 (2005).
ENIGMA on social media: